The economics of clinical documentation technology is an important consideration as the healthcare industry undergoes a digital transformation. Clinical documentation solutions are emerging as critical tools for driving financial performance. However, navigating the economics of implementing and optimizing these technologies can be challenging for healthcare administrators and financial executives.
This article aims to provide a comprehensive exploration of the economic aspects of clinical documentation technology, including cost-benefit analysis, return on investment case studies, and the impact on reimbursements and revenue cycle management.
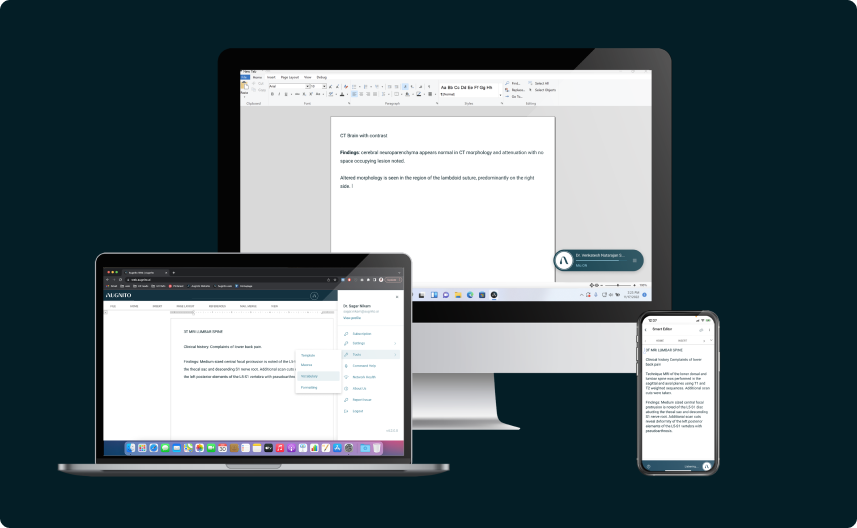
Specifically, we will examine how advanced solutions utilizing artificial intelligence and health informatics can optimize patient care while also improving the accuracy and efficiency of the clinical note documentation process. Understanding these dynamics is essential for healthcare leaders looking to capitalize on the financial promise of clinical documentation technology while also enhancing the quality of patient care.
The Evolving Role of Technology in the Economics of Clinical Documentation
Clinical documentation encompasses the written records of patient conditions, treatments, and outcomes that are vital for quality care delivery. Traditionally a manual process relying on paper charts and transcription, advances in healthcare IT have automated and optimized documentation through solutions like electronic health records (EHRs), computer-assisted coding (CAC), speech recognition, and clinical documentation improvement (CDI).
With tight budgets and competing priorities, healthcare financial executives must keenly understand the economics of clinical documentation technology, specifically how artificial intelligence and AI applications can optimize the medical record process to drive revenues and reduce costs across the healthcare system. The metrics here uncover the dollars-and-cents impact of this technology adoption to inform data-driven decision-making on investments into documentation improvement powered by AI.
Cost-Benefit Analysis of Clinical Documentation Systems
Determining true return on investment requires an objective breakdown of implementation and ongoing costs compared to efficiency gains, time savings, and revenue gains.
Here are the key aspects of the cost-benefit equation:
Initial Costs
- Software licensing/subscription fees
- Interface build-outs and data integration
- Hardware upgrades or data center expansion
- Implementation team training and support
Ongoing Expenses
- Software upgrades and application management
- IT infrastructure and data security maintenance
- End-user training and change management
Efficiency Gains
- Automated documentation workflows
- Reduced documentation time for clinicians
- Streamlined coding and claims processes.
Revenue Impact
- Improved documentation accuracy for optimized reimbursement
- Reduced claim denials and payment delays
- Higher coder productivity and throughput
The global Electronic Health Records (EHR) market size was valued at USD 24,680.0 million in 2024 and is expected to expand at a CAGR of 5.02%.
Real-World Return on Investment Case Studies
Beyond projected metrics, real-world implementation case studies offer tangible validation of achieving ROI. Here are examples of healthcare institutions realizing material financial returns from their documentation technology investments:
Primary Care Practices’ EHR Implementation
A mixed-methods study conducted on the use of electronic health records (EHR) in primary care practices revealed that these clinics typically recovered their investment in EHR systems within an average of 6.2 months. The study found that the implementation of EHR systems led to improved active-patients-to-clinician-FTE and active-patients-to-clinical-staff ratios, which in turn increased the clinic’s net revenue.
OrthoIndy’s Use of Ambient Clinical Intelligence
OrthoIndy, an orthopedic clinic based in Indianapolis, implemented ambient clinical intelligence (ACI) to boost efficiency in its operations. ACI, a form of AI technology, was used to automate the documentation process, allowing physicians to focus more on patient care. While specific financial figures are not provided in the search results, the case study highlights the potential of ACI to transform care delivery and significantly impact the financial performance of healthcare providers.
These case studies demonstrate that clinical documentation technology, when effectively implemented, can deliver significant and sustained ROI across diverse healthcare institutions. The key is gaining user adoption to realize maximum financial impact.
As stated by the CFO of a leading regional health system, “Having the optimal technology is just the starting point. We worked extensively with frontline clinicians and coders to ensure the solutions delivered value and efficiency to their daily work. This is what ultimately moved the needle to achieve impressive ROI across our hospitals.”
Impact on Reimbursements and Revenue Cycles
The downstream revenue cycle implications of accurate and timely documentation are profound. Some key interdependencies that impact financial outcomes:
Reimbursement Rates: Improved documentation capture of diagnosis codes, severity levels, and quality measures leads to higher reimbursement rates and less revenue leakage. Solutions leveraging artificial intelligence to extract insights from health information can assist healthcare professionals in optimizing documentation.
Claims Processing: Structured data and streamlined workflows reduce claims errors and denials for faster processing. This improves cash flow. Health systems adopting documentation technologies see faster claims reimbursement.
Revenue Leakage: Tighter integration between documentation and coding reduces missed charges and unpaid claims, plugging revenue leakage.
Compliance: Consistent clinical documentation practices improve audit readiness for regulatory requirements, avoiding financial penalties.
Savings from Transcription and Scribes
Many healthcare organizations rely extensively on medical transcription or scribes to manage documentation, which carries significant financial burdens. Technology solutions that automate workflows can substantially reduce or eliminate these costs over time.
The in-house operational expense for medical transcriptions could cost a hospital or a healthcare provider approximately $0.22 per line, compared to $0.08 per line when outsourced.
Likewise, The average hourly wage for a medical scribe in the United States is around $18, with a typical range between $15 and $20. In New York, the average salary for a medical scribe is $20.17 per hour. Some services offer virtual scribes for around $14-$16 per hour.
Transitioning even partially away from manual documentation processes towards technology-enabled clinician self-service can deliver considerable cost savings. Any reduction in transcription or scribe utilization has an immediate and material financial benefit.
Key Metrics and Benchmarks for Success
While clinical documentation technology delivers clear qualitative benefits, financial executives expect to see quantitative outcomes. Objective metrics are essential for evaluating success.
Here are suggested key performance indicators (KPIs) to precisely track financial impact:
- Expense Reduction: Decreased transcription, scribe, and outsourced coding expenses.
- Revenue Per Encounter: Increased revenue capture tied to each patient visit
- Reimbursement Rates: Growth in reimbursement dollars per filed claim
- ROI Timeline: Months to break even on implementation costs
- Claim Denials: Reduced percentage of claims rejected or denied
Health policy and health economics experts advise healthcare professionals and administrators to closely monitor these metrics to optimize medical services revenues, costs, and quality of care. Assessing clinical documentation technology investments through these healthcare setting KPIs can inform data-driven decision-making.
Industry benchmarks for these KPIs include:
- 2-4X return on investment in 2-3 years
- 10-20% increased revenue per encounter
- 30-50% reduction in claim denial rates
Setting targets aligned to benchmarks enables accurate success measurement. The key is pairing financial metrics with clinical usage data to correlate system adoption to outcomes. Ongoing performance monitoring also allows for optimization towards achieving better economics of clinical documentation.
Overcoming Financial Challenges
Despite compelling cost-benefit data, securing the initial budget for documentation system investments poses challenges in healthcare’s fiscal reality. Some proven arguments to overcome financial objections include:
- Future-Proofing Goals: Clinical documentation is the underpinning for digital growth strategies centered on analytics, interoperability, and patient engagement.
- Market Competition: Keeping pace with technology adoption is essential to maintaining reputation, market share, and public perception.
- Risk Mitigation: Updated systems proactively address security, privacy, and patient safety risks.
Budget constraints can be overcome by value-focused pilots. Small use case deployments allow for proving ROI potential before large-scale investment. External funding mechanisms like shared savings partnerships with vendors also help ease budget pressures.
Looking Ahead: The Future of Clinical Documentation Technology Economics
While this article outlines the current financial landscape, emerging innovations will reshape the economics of clinical documentation technology.
Key trends to watch include:
- Predictive Coding: Machine learning will enable automated diagnosis recommendations and coding, driving efficiency.
- Artificial Intelligence-based Medical Speech Recognition: Continued accuracy improvements will expand clinician adoption, reducing transcription costs.
- Blockchain: Distributed ledger solutions could streamline revenue cycle events like claim adjudication.
- Consumerization: Patient-generated documentation will complement clinical records with diverse data.
These innovations will compel new analysis of cost inputs and revenue opportunities. Financial executives staying abreast of the latest developments will be best positioned to capitalize on the economics of clinical documentation technology.
In Summary: The Dollars and Sense Economics of Clinical Documentation Technology
This exploration of the financial considerations around implementing and optimizing clinical documentation technology equips healthcare financial executives to make informed decisions grounded in real-world evidence.
With pressures mounting to control expenses amid shrinking reimbursements, documentation technology represents a pathway to material expense reduction and revenue gains without compromising care quality. The combination of cost-benefit fundamentals outlined here, paired with emerging innovations like artificial intelligence, creates a compelling value proposition for healthcare administrators to invest confidently.
Tracking metrics like lowered transcription costs, increased revenue per encounter, higher reimbursement rates and accelerated claims processing against industry benchmarks enables precise measurement of the financial success of clinical documentation technology. With the right technology foundation and optimization strategy focused on user adoption, healthcare institutions can transform the economics of clinical documentation from a cost center to a revenue driver. Understanding the dollars-and-cents dynamics and downstream revenue cycle impact is key to capitalizing on the promise of these solutions.