Physician burnout has surfaced as a critical issue with modern healthcare setups, with studies indicating that up to 42-63% of physicians are battling with burnout symptoms, such as emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. This alarming trend not only threatens the wellbeing of healthcare providers but also negatively impacts patient care and clinical outcomes. Factors like intense workloads, challenging interpersonal dynamics, and varying autonomy levels contribute to an environment where physician burnout thrives. Despite these obstacles, resilience emerges as a powerful tool, offering a glimmer of hope for those immersed in the demanding world of medical professions.
Our collective resolve to address this mounting concern gave rise to the expansion of the “Triple Aim of Health Care” to the “Quadruple Aim”, underscoring clinician wellbeing as a pillar equally crucial as patient care.
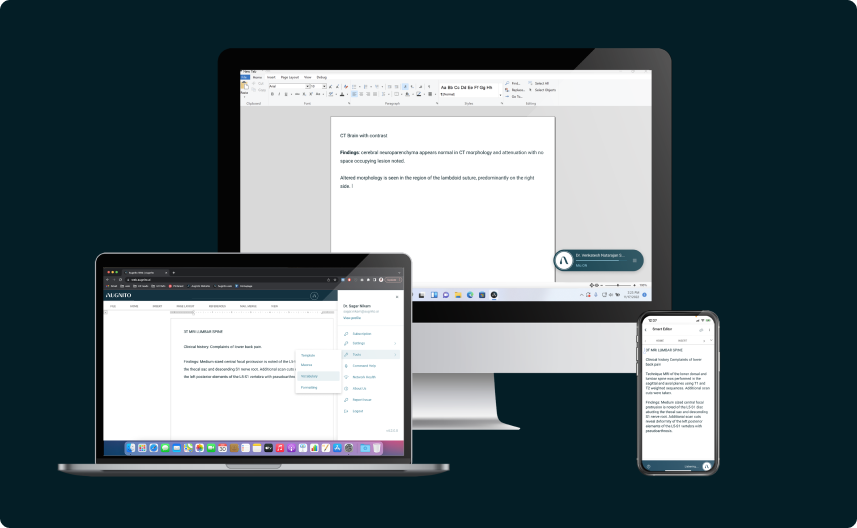
In this article, we will delve into doctor resilience training, a formidable strategy that can potentially “inoculate” individuals against the inherent pressures of the medical landscape. We will explore resources for physician wellbeing and burnout prevention, unveiling organizational changes that streamline inefficiencies and mitigate excessive demands. Emphasizing emotional intelligence and championing wellness programs, our journey will equip physicians with tools for managing emotions in a stressful work environment.
In acknowledging the dire necessity for physician wellness programs, we strive to craft a new narrative—one where reducing physician stress is paramount, embedded within medical education to nurture a workforce that thrives amidst adversity.
The Prevalence of Burnout Among Healthcare Providers
The COVID-19 pandemic has undoubtedly intensified stress within the healthcare workforce, triggering a rise in physician burnout statistics. The leading contributors to rising burnout rates among healthcare workers during COVID-19 include increased workload and emotional exhaustion from difficult work conditions – caring for extremely ill patients, facing supply and resource constraints, and witnessing immense suffering and loss of life. Many healthcare workers also report struggles with mental health issues like anxiety, insomnia and PTSD symptoms in the wake of intensive pandemic response.
The intent to leave one’s job due to burnout is alarmingly high, with 24.3% of physicians contemplating such a decision within the next two years. Nurses are reporting the highest rates of intending to leave their jobs (41.0%), a statistic that could significantly affect patient care continuity. Work overload, a strong and independent predictor of burnout, has been reported by 47.4% of non-physician and non-nurse clinical staff, highlighting the need for systemic approaches to reduce physician stress, such as ensuring sustainable compensation and providing adequate mental and physical health safeguards.
Burnout among clinicians, particularly physicians, is a significant issue due to the demanding nature of healthcare environments, leading to reduced access to care, threats to patient safety, and impaired care quality. Factors such as time pressures, chaotic environments, low control over work pace, and unfavorable organizational culture are strongly associated with clinician burnout. The implementation of electronic health records, while intended to streamline care, has also contributed to this issue. However, interventions such as scheduling regular provider meetings, enhancing team functioning, and having medical assistants enter patient data can improve clinician outcomes and reduce burnout, serving as a testament to the importance of physician wellness programs and the cultivation of emotional intelligence for high-stress medical careers.
The Consequences of Burnout
Physician burnout is a complex syndrome characterized by emotional exhaustion, cynicism, and a diminished sense of personal accomplishment. Examining the repercussions of burnout, it’s evident that its effects extend beyond the individual, permeating the entire healthcare ecosystem. Around one in three physicians may suffer from burnout at any time, which can profoundly disrupt their wellbeing and compromise the quality of care they provide.
The personal repercussions for healthcare providers are profound and include:
- Substance Abuse: An increased risk as clinicians attempt to cope with the high levels of stress.
- Relationship Strain: Increased friction and higher rates of divorce due to the emotional toll of burnout.
- Mental Health Issues: Heightened levels of unhappiness, anxiety, depression, and isolation, with a higher prevalence of depressive disorders and sleep disorders directly linked to burnout.
On a professional level, the consequences are equally severe and include:
- Patient Care: Lower patient satisfaction and impaired quality of care.
- Clinical Errors: Increased medical errors and higher rates of malpractice suits.
- Workforce Dynamics: Decreased job satisfaction, absenteeism, and high turnover in personnel.
These outcomes not only affect the individual healthcare worker but also lead to a decline in the overall quality of healthcare systems. Poor adherence to guidelines, communication breakdowns, and compromised patient safety are indirect effects of burnout that can erode the trust and efficacy of healthcare delivery.
To combat these issues, it’s crucial to implement measures focusing on both individual and organizational levels. For healthcare workers, recommended strategies include engaging in self-care practices like physical activity, balanced diet, and good sleep hygiene. Additionally, fostering job satisfaction and self-awareness through reflective practices and small group discussions can be beneficial. On an organizational scale, building resilience among frontline workers is key, which can be achieved by supporting effective communication, providing professional psychosocial support, and setting reasonable limits on shift durations and frontline exposure periods.
By integrating these strategies into our approach, we aim to address the critical issue of physician burnout, enhancing resources for physician wellbeing and burnout prevention, and ultimately fostering a healthier work environment that allows for managing emotions in a stressful work environment more effectively.
Preventing and Reversing Burnout Through Resilience
It is apparent that resilience is crucial in both preventing and mitigating this condition, with a significant portion of physicians meeting the criteria for burnout, the demand for effective interventions is clear. Women physicians, in particular, are at a greater burnout risk than their male colleagues.
Burnout often stems from unmet expectations and systemic failures within the medical practice environment. While doctor resilience training can empower individuals to manage the occupational suffering inherent to their roles, it is crucial to recognize that systemic improvements are necessary to address avoidable suffering caused by organizational pathologies.
To enhance the resilience of healthcare providers, several competency goals have been identified:
- Creating Connection: Establishing a supportive environment where physicians can connect with peers and mentors.
- Mindful Self-Awareness: Practicing mindfulness to stay present and engaged, thus reducing stress levels.
- Cognitive Reappraisal Skills: Learning to reframe negative thoughts and challenges in a more positive light.
- Holistic Self-Care and Positivity: Encouraging a balanced lifestyle that includes physical, emotional, and spiritual well-being.
- Empathy Practice: Developing the ability to understand and share the feelings of others, enhancing patient-physician relationships.
Implementing these goals through structured programs has shown promising results. A program that incorporated mindfulness, appreciative inquiry, and narrative techniques successfully prevented burnout in primary care physicians, enhancing their resilience and developing their sense of insight.
Moreover, for practicing physicians, self-reflection questions and action steps focused on the ‘resiliency triad’ can be transformative:
- Aligning Practice with Values: Ensuring that daily activities and responsibilities reflect personal and professional values.
- Providing Self-Care: Engaging in regular physical activity, balanced nutrition, and adequate rest.
- Developing Insight: Gaining a deeper understanding of one’s behaviors and motivations to foster emotional intelligence for high-stress medical careers.
By incorporating these strategies into physician wellness programs, we can offer resources for physician wellbeing and burnout prevention, ultimately reducing physician stress and managing emotions in a stressful work environment more effectively.
Strategies for Cultivating Resilience
In our ongoing efforts to mitigate physician burnout, we focus on nurturing resilience among healthcare workers (HCWs). Resilience, the capacity to recover from adversity, involves aspects such as moral purpose, connections, collaboration, organizational culture, character, and self-care. This quality is especially vital in high-pressure settings like healthcare, more so during crises like the COVID-19 pandemic. We propose strategic methods to cultivate this essential trait:
- Fostering Emotional Intelligence:
-
- Cultivate an environment that encourages HCWs to recognize and understand their emotions and those of others.
-
- Implement training that guides emotions through thinking and behavior, rather than being led by emotions, which is essential for managing emotions in a stressful work environment.
-
- Creating Supportive Organizational Cultures:
-
- Develop systems that measure and create resilience among HCWs, considering them as a defense against failure.
-
- Health care leaders must build long-term team sustainability, understanding organizational limitations and the necessity of care quantity in a fee-for-service world.
-
- Structured Resilience Programs:
-
- Integrate explicit programs like web-based cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) to help prevent adverse mental health outcomes.
-
- Encourage participation in resilience courses for health professionals to maintain physical and emotional health and nurture social relationships, thus creating a more resilient workforce.
-
By embedding these strategies within our physician wellness programs and resources for physician wellbeing and burnout prevention, we not only strive to reduce physician stress but also aim to enhance the overall quality of healthcare delivery. Through the concerted efforts of both individuals and organizations, we can construct a robust framework that supports doctor resilience training and fosters a culture where emotional intelligence for high-stress medical careers is not just an aspiration but a reality.
Implementing Organizational Change
Addressing physician burnout necessitates an imperative shift towards organizational change that supports healthcare provider wellbeing. Our continuous advocacy for doctor resilience training and resources for physician wellbeing underscores the need for systemic and organizational strategies to alleviate physician stress and aid in managing emotions in a stressful work environment.
Teamwork and Support Structures:
-
- Expanding the roles of medical assistants has also been shown to enhance professional fulfillment and practice satisfaction, demonstrating that well-structured teamwork can be a cornerstone in physician wellness programs.
-
- Implementing team-based care models and encouraging communication among physicians has shown to be effective. In fact, out of nine studies focusing on the use of scribes, seven reported significant improvements in clinic workflow efficiencies, highlighting the positive impact on reducing physician burnout.
Redesigning Work Systems:
-
- Health care organizations are encouraged to adopt fundamental principles that prioritize the prevention and reduction of burnout, while simultaneously promoting wellbeing. This could involve modifications to work processes, such as shortened shifts, rotation lengths, and duty hour requirements, as well as addressing productivity targets and optimizing the use of electronic health records (EHR).
-
- A comprehensive approach to redesigning work systems includes addressing the four pivotal areas identified in the review: Teamwork, Time, Transitions, and Technology. For instance, providing full-time clerical support to manage physician order entry in primary care has been shown to decrease self-reported burnout by 29%, from 43% to 14%.
Cultural and Value Alignment:
-
- Organizational leadership is tasked with the critical role of creating a culture of wellness. This involves demonstrating commitment, modeling change, and addressing burnout at a systemic level. By articulating values and missions, the physician leadership can guide decision-making, ensuring it aligns with the wellbeing of their employees.
-
- Providing flexibility in work effort, work hour distribution, and start times can grant physicians greater control and autonomy, which is a significant factor in mitigating burnout. Furthermore, fostering social support through mentorship programs, social events, and team-building exercises can enhance relationships within the work environment and contribute to a community that supports emotional intelligence for high-stress medical careers.
By integrating these evidence-based interventions, we aim to construct a robust framework that not only supports the individual healthcare provider but also strengthens the healthcare system as a whole, ensuring that physicians have the resources and support they need to thrive in their high-stress roles.
Conclusion
As we reflect on the journey through the daunting landscape of physician burnout, it is apparent that fostering resilience is not merely an option but a necessity for the wellbeing of healthcare professionals and the public health. Our exploration has illuminated the critical role that emotional intelligence, supportive work environments, and comprehensive wellness programs play in combating the rigors of medical practice. The shared responsibility between individuals and institutions to effectuate change is undeniable, and the implementation of these programs has the manifold benefit of enhancing physician satisfaction and patient care quality.
Emerging from the shadows of burnout, there is a hopeful vision of a healthcare system that prioritizes the fortitude of its caregivers alongside the safety and satisfaction of its recipients. It beckons a future where medicine is practiced with vigor, compassion is sustained, and resilience is ingrained in the very fabric of medical culture. With collective commitment and actionable strategies, the path to a reinvigorated workforce is not only conceivable but well within our grasp.